Background/Purpose: Multisystem inflammatory syndrome in children (MIS-C) is a rare consequence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). MIS-C shares features with common infectious and inflammatory syndromes, and differentiation early in the disease course can be difficult. We aimed to develop a diagnostic prediction model using clinical, laboratory, and cardiac features within the first 24 hours of presentation to distinguish children with MIS-C from those with alternative diagnoses.
Methods: Data were obtained by retrospective chart review of children (≤20 years) admitted to Vanderbilt Children’s Hospital and evaluated for MIS-C using our institutional algorithm between June 10, 2020 – April 8, 2021. Standardized clinical, laboratory, and cardiac characteristics were collected on each child during the first 24 hours of hospital presentation. Our outcome was defined as clinically diagnosed MIS-C, which was determined by the child’s primary service and retrospectively reviewed and confirmed by both a Pediatric Rheumatologist and Pediatric Infectious Disease physician. Candidate predictors were selected a priori and were examined for collinearity Spearman correlations. Logistic regression with bootstrapped backward selection was used to identify the most important predictors for MIS-C. Variables selected in ≥80% of 500 bootstraps were included in the final model. Discrimination was quantified with C-index and calibration was assessed using a calibration plot. Internal validation with bootstrap resampling was used to estimate optimism-corrected performance measures.
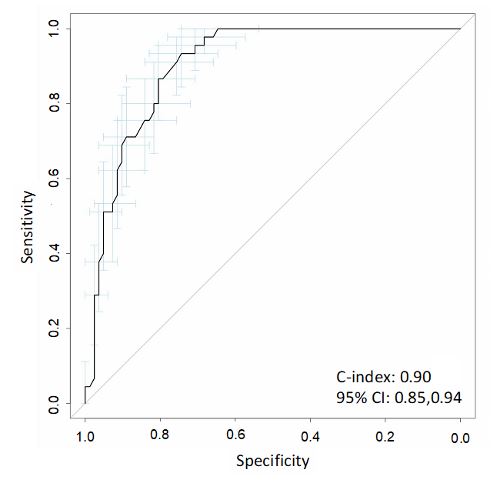
Results: During the study period, 127 children were admitted to our hospital with concern and evaluation for MIS-C. We identified clinical, lab, and cardiac features that distinguished those with MIS-C (n=45) from those without (n=82). We used statistically distinct variables to build a risk prediction model. Four predictors were included in our final model: hypotension (defined as requiring fluid resuscitation, vasopressor support or blood pressure less than 10th percentile for age, height and sex), abdominal pain, rash, and serum sodium (mmol/L). The model showed excellent discrimination with c-index of 0.90 (95% CI: 0.85, 0.94; Figure 1). The model has good calibration but has slight departure between 20-40% probability (optimism-corrected slope: 0.93; optimism-corrected intercept: -0.04; Figure 2).
Conclusion: We used early clinical and laboratory features to inform the design of a clinical diagnostic prediction model with excellent discrimination to assist clinicians in distinguishing patients with MIS-C from those without. We plan to test this model with external and prospective validation.
The post A Prediction Model to Distinguish Patients with Multisystem Inflammatory Syndrome in Children appeared first on ACR Meeting Abstracts.